Abstract
Chronic lymphocytic leukemia (CLL) is a complex disease with very heterogeneous biological and clinical behavior. The disease may have a stable course but also become aggressive, with frequent relapses, or even transform into an aggressive lymphoma, typically diffuse large B-cell lymphoma (DLBCL), known as Richter transformation (RT). The generation of adequate pre-clinical mouse models fully reflecting tumor biology has not yet been successfully achieved. The establishment of patient-derived xenograft (PDX) from primary CLL can contribute to understand the pathogenesis of the disease and to assess the efficacy of new therapies.
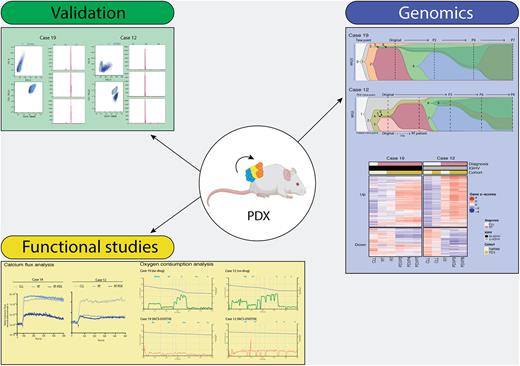
To develop PDXs, we xenotransplanted cryopreserved samples from 11 patients with CLL or clonally-related RT into immunocompromised NOD/SCID/gamma(c)(null) (NSG) mice subcutaneously. Once tumor engrafted, cells were collected and reinjected. This process was repeated several times (6 passages on average) until the generation of stable models. Under these conditions, we have generated two PDXs from peripheral blood primary samples of a RT (case 19) and CLL (case 12). Clonal relationship of the primary tumor with the PDXs was performed by flow cytometry analyses of CD19+/CD5+ population and detection of the rearrangement of the immunoglobulin heavy chain. Whole-genome sequencing (WGS) and bulk RNA-seq studies of primary CLL samples and PDXs (three different time points through PDX development) were performed. WGS revealed that the PDX of case 19 (RT) maintained the genetic alterations of the RT primary sample (NOTCH1, SF3B1, TP53 and CDKN2A/B) and acquired amplifications of MAP3K7, MYC and BCL2 leading to overexpression of the target genes, which were confirmed by fluorescence in situ hybridization (FISH) and/or western blot. Single cell RNA sequencing studies of these original cases (Nadeu F. et al. Nature Medicine in press) together with FISH confirmed that these alterations observed in PDX samples were already present in a minor subclone of the initial RT sample, indicating the heterogeneous genomic evolution of RT arising from preexisting small subclones.
In case 12, although the PDX was generated from a primary CLL sample carrying NOTCH1, MGA and XPO1 mutations, the engrafted subclone carried most genetic alterations acquired in the RT subclone expanding in the patient five months after sampling, including SF3B1 and SPEN alterations, among others. In addition, the RT subclone expanding in the PDX also harbored alterations in CARD11 and PIM1. The evolution of the CLL to RT in this PDX largely mimicked the trajectory of the RT observed in the patient.
RNA-seq analysis of these PDXs showed a similar expression profile as described in RT samples, characterized by a decrease of the B cell receptor (BCR) signaling and increase of the oxidative phosphorylation (OXPHOS) pathways. These results were validated by functional in vitro experiments. PDXs showed higher oxygen consumption at routine respiration and electron transfer system capacity than the parental samples and a reduction of BCR signaling determined by analysis of calcium flux. As both patients developed RT under ibrutinib treatment, we tested the effect of this drug in our PDXs and primary samples. We found than both PDXs were resistant to ibrutinib and no mutations in BTK or PLCG were detected. These findings are of special interest in case 12, because our PDX was primary resistant to ibrutinib and the original CLL sample was sensitive to the drug, suggesting that resistance to this drug may be acquired independently of its exposure. Finally, we observed that RT cells were resistant to venetoclax, but this resistance could be circumvented by the incubation of cells in combination with the OXPHOS inhibitor IACS-010759.
These results highlight the molecular heterogeneity of CLL and RT and confirm that aggressive RT subclones might be present in early stages of the disease. We showed that PDX models represent a useful tool for studies of clonal evolution as they recapitulate the evolution of CLL towards RT. The OXPHOShigh-BCRlow signaling axis observed in RT could contribute to their low response to BCR inhibitors. We propose that targeting OXPHOS in combination with venetoclax might be a potential targeted therapy in RT patients. Altogether, these models will facilitate the development of new therapeutic opportunities for patients with RT.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal